We are living in unprecedented times as a result of COVID-19. Effective communication is essential at all times – but especially now. Everyone needs to understand what is happening and everyone needs to be able to express needs and wants, and obtain important information.
This can be an especially frightening and stressful time for individuals who face significant communication challenges. This group might include individuals with
- developmental disabilities (e.g., autism spectrum disorder, cerebral palsy, Down syndrome, intellectual developmental disabilities);
- acquired conditions (e.g., traumatic brain injury, spinal cord injury, stroke);
- degenerative conditions (e.g., ALS, dementia) and
- temporary conditions such as intubation to support breathing as a result of COVID-19, surgery, or other causes.

These individuals may require augmentative and alternative communication (AAC) supports especially at challenging times such as these. The following are some tips and resources for individuals with complex communication needs and their families and caregivers at this difficult time.
Preparing in advance – just in case

If you are someone who uses AAC, or someone who cares for someone who has complex communication needs, it is important to be prepared to ensure that communication needs are met.
- Be sure to identify a group of individuals who can provide support and assistance should this be necessary. Remember that a primary caregiver may become ill and may be unable to support the communication of the individual who has complex communication needs. Be sure that there is a network of other people who can step in to provide support as required. Make sure each person knows their roles and responsibilities. Keep everyone updated using social media or other means.
- Prepare communication support materials to help with comprehension and expression. Make sure these are “ready to go” in case the individual who relies on AAC becomes ill and requires medical assistance. Be sure to include low-tech, nonelectronic options as it may not be possible to access and use technologies. There are some ideas and suggestions listed below.
- Prepare a medical or health passport in advance that includes all critical health information including medical conditions, medications, current medical team, contact information, etc. Make sure that this is easily located to share with medical personnel.
- Prepare instructions for medical staff or other new communication partners explaining communication techniques as well as positioning and daily care requirements. Use simple clear language. Provide photos if possible to illustrate or include videos demonstrating techniques.
- Hospitals and other medical facilities are required to provide supports and services to ensure effective communication with patients. They cannot exclude or treat patients differently because of their disability.
Supporting understanding of COVID-19

If you care for someone with complex communication needs who has difficulty understanding spoken communication, here are some pointers and resources:
- Use short sentences to explain the situation. Speak slowly.
- Use familiar vocabulary. Relate information to familiar experiences. Use concrete terms.
- Use visual supports to assist with understanding.
- Use gestures or demonstrate instructions as you speak
- For example, demonstrate washing hands, staying at least 6 feet away from people, wearing a mask
- Write down key words as you speak to support understanding
- Show photos as you explain
- For example, show a photo of an ambulance or a medical worker in protective gear as you explain what happens when people go to the hospital
- Provide a visual schedule of the steps that will occur
- Use a social story to explain what will happen
- For example, use pictures and photos to tell a story of what will happen when the individual goes for a COVID-19 test
- Show a video to explain what is going to happen
- Use gestures or demonstrate instructions as you speak
- Repeat information regularly as required to support understanding and learning.
Supporting expressive communication

If you are someone who uses AAC or someone who cares for someone who cannot rely on speech to communicate with others, here are some pointers and resources:
- Establish clear yes/ no signals.
- Yes /no signals might include a head nod or shake, thumbs up or down, looking up or looking down. These signals should be easy to produce and easy to recognize.
- Prepare personalized low-tech nonelectronic communication supports. Depending on the individual’s needs and skills, these might include
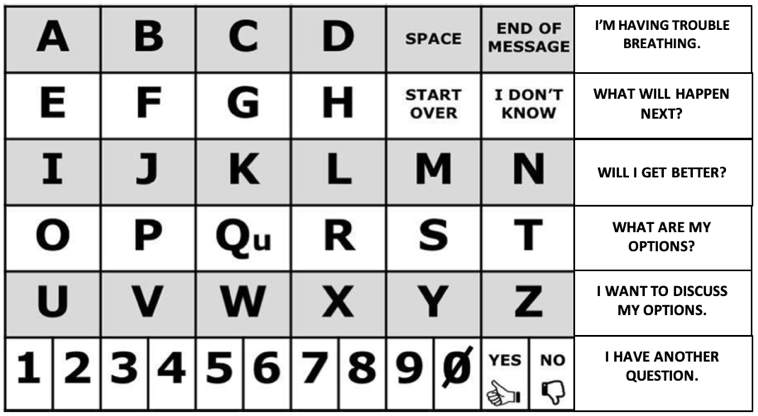
- Alphabet board with high importance messages
- Word board to express medical needs and wants and ask questions
- Communication board of pictures or photos to express medical needs and wants
- Dry erase board
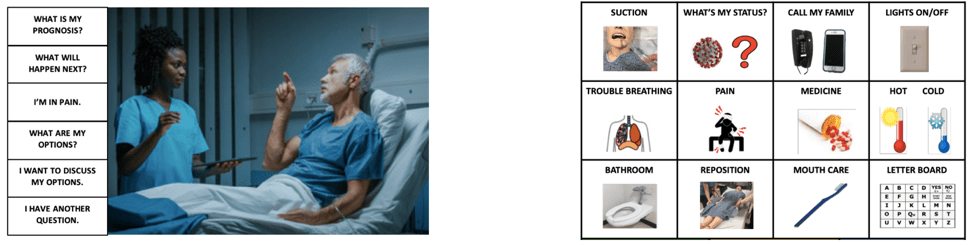
A personalized grid-display with basic vocabulary (right) (from PPC)
- Practice using these in advance so that they are familiar.
- Prepare instructions for medical staff or other new communication partners. Explain communication techniques (e.g., asking appropriate questions, waiting, confirming understanding). The instructions should also include information on positioning and daily care requirements. Keep the instructions as short as possible. Use simple clear language. Provide photos to illustrate or include videos demonstrating techniques.
If you are a healthcare provider caring for someone who cannot speak, here are some pointers and resources

- Always stand where the patient can see you. Be sure the patient can hear you.
- If the patient had a pre-existing disability,
- Check to see if they have a health passport with critical medical information.
- Check to see how they communicate (e.g., do they have an alphabet board, picture board, or iPad that they use to express themselves).
- Check to see if they have instructions for unfamiliar communication partners to explain how to communicate effectively.
- If the patient is temporarily unable to speak due to intubation or other medical treatment or if you are unable to locate the patient’s communication supports,
- Establish yes /no signals
- Yes /no responses might include a head nod or shake, thumbs up or down, looking up or looking down
- Ask “How do you communicate ‘no’?” and observe carefully. Repeat for ‘yes’ signal
- Once these signals are established, record them in the patient’s medical chart and post them bedside for other healthcare providers
- Ask one question at a time and wait for the patient to respond. Provide choices one at a time.
- For example, ask the patient “Are you in pain?”
- If the patient looks up to communicate “yes”, then ask questions one at a time to identify the location of the pain. Wait after each question.
- For example, ask “Does your head hurt?” and wait for a response. “Does your chest hurt?” and wait for a response.
- Confirm with the patient that you understood their response correctly
- Explain to the patient what is happening. Use gestures and demonstrations or show pictures to support understanding as needed. Confirm that they have understood.
- Provide a communication board with the alphabet, written words, pictures, or photos so that the patient can communicate with you. Ask the patient to spell messages or to point to written words or pictures to communicate needs.
- Establish yes /no signals
For additional resources to support communication, please visit
- Autism Speaks
- Autism Society
- Alzheimer’s Association
- Boston Children’s Hospital–My Hospital Planning Packet: Prepare for a hospital visit during the COVID-19 pandemic
- Communication Rights Toolkit from CommunicationFIRST
- Patient Provider Communication Network
- PrAACtical Resources: Dealing with the Covid-19 Pandemic
- TechOWL–Institute on Disabilities at Temple University
- The National Down Syndrome Society
- Tobii Dynavox
- UNC Frank Porter Graham Child Development Institute Autism Team
For further information on COVID-19, please visit the CDC website.